What is Hormone Replacement Therapy (HRT)?

Hormone Replacement Therapy (HRT) - The Facts
The menopause is a normal life event for women, not an illness or a medical condition. However, the effects of the menopause often have a negative impact on a woman’s wellbeing and quality of life, and are frequently underestimated by both women and their doctors. Furthermore, the low estrogen levels and other biological changes that occur in menopausal women are also associated with an increased risk of cardiovascular disease, osteoporosis, type 2 diabetes, and dementia.
Around 75% of menopausal women experience symptoms, with around one-third of these experiencing severe symptoms which are having a negative effect on their lives, both at home and at work.
Peri-menopause and menopause are finally being taken seriously and enjoying some attention from the media, the medical profession and government. Experts such as Dr Louise Newson are working tirelessly to provide clear, evidence based information to women, to clear up some of the confusion and dispel the myths about symptoms and the safety of Hormone Replacement Therapy. The channel 4 documentary presented by Davina McCall and produced by Kate Muir made great strides in helping to educate and inform women
Over the past two decades, there has been a huge amount of confusion regarding Hormone Replacement Therapy (HRT). But clearer, evidence-based guidelines are now available to ensure women have individualised care and treatment for their perimenopause and menopause. However, many women and healthcare professionals are still worried about the perceived risks of Hormone Replacement Therapy (HRT). Much of the negativity regarding HRT stems from the misinterpretation of the Women’s Health Initiative (WHI) study in 2002, which led to a worldwide reduction in HRT use. The subsequent sub-analysis of this study revealed reassuring and positive results to support the use of HRT, especially in younger women. Other research has supported the National Institute for Health and Care Excellence menopause guidelines that the benefits of HRT outweigh the risks in the majority of women.
This blog sets out the known facts about HRT and is written specifically to inform women who wish to know about HRT. However, we strongly recommend that you should discuss with your doctor both the benefits and the risks of HRT on an individual basis.
HRT - History, Benefits & Risks
Hormone Replacement Therapy (HRT) was first available in the 1940s but became more widely used in the 1960s, creating a revolution in the management of the menopause. HRT was prescribed commonly to menopausal women for the relief of their symptoms such as hot flushes, night sweats, sleep disturbances, psychological and genito-urinary problems – urinary frequency and vaginal dryness – and for the prevention of osteoporosis. In the 1990s two of the largest studies of HRT users were undertaken, one clinical randomised trial in the USA [Women’s Health Initiative (WHI)] and one observational questionnaire study in the UK [the Million Women Study (MWS)]. The published results of these two studies during 2002 and 2003 raised concerns regarding the safety of HRT. These safety concerns revolved around two main issues: 1) that the extended use of HRT may increase the risk of breast cancer and 2) that the use of Hormone Replacement Therapy may increase the risk of heart disease.
The results of the studies received wide publicity, creating panic amongst some users and new guidance for doctors on prescribing. After the results were published, the UK regulatory authorities issued an urgent safety restriction about HRT, recommending that doctors should prescribe the lowest effective dose for symptom relief, should use it only as a second line treatment for the prevention of osteoporosis, and advised against its use in asymptomatic postmenopausal women. There remains widespread confusion and uncertainty amongst both doctors and HRT users. Many doctors stopped prescribing HRT and many women abandoned HRT immediately, with a return of their menopausal symptoms.
The number of women taking HRT fell by 66%, which has not changed so that now after more than 10 years, there has been almost a generation of women who have mostly been denied the opportunity of improved quality of life during their menopausal years. The women studied in the WHI were North American women in their mid-sixties, often overweight and thus totally unrepresentative of women in the UK for whom HRT might be considered suitable. These would usually be around the age of the menopause, namely 45-55 years. It should also be appreciated that, in a surprising turnabout, subsequent publication of the full WHI results showed the apparent increased risk for breast cancer was only found in those who had taken HRT before entering the study.
The WHI long-term randomised clinical trials published in 2020 showed a significant reduction in breast cancer diagnosis and mortality in women using estrogen only HRT. Like the NICE guideline conclusions, they found that women on combined estrogen and progestogen containing HRT had an increased risk of breast cancer diagnosis but no significant increase in mortality. The Collaborative Group on Hormonal Factors in breast cancer 2019 reported that obesity attenuated the absolute and the relative excess breast cancer risk associated with both estrogen only and combined HRT. Large observational trial data suggest that micronized progesterone and dydrogesterone are likely to be associated with a lower risk of breast cancer compared to that seen with other progestogens.
Hormone Replacement Therapy remains licensed for osteoporosis prevention and can be considered the treatment of choice for women starting treatment below age 60 years, and especially for those with a premature menopause. Women on HRT should be re-assessed by their doctor at least annually. For some women, long-term use of HRT may be necessary for continued symptom relief and quality of life. Many health centres and practices have a doctor with a special interest in postmenopausal health. These specialist GPs will know the up-to-date recommendations for prescribing HRT. They may also be members of the British Menopause Society, the professional partner to Women’s Health Concern, and therefore have access to its latest literature, studies and training. However, if your family doctor does not have sufficient knowledge of the current situation concerning the benefits and risks of HRT and many have lost confidence in prescribing because of the recent scares, then it is your right to request advice from a local Menopause clinic or a specialist with known expertise in menopausal health
So, what is Hormone Replacement Therapy?
Hormone replacement therapy (HRT) is used to relieve women of symptoms associated with the menopause. The aim of HRT is to restore female hormone levels, which in turn can bring relief to many women.
Oestrogen and progesterone are female hormones that play important roles in a woman’s body. Falling levels cause a range of physical and emotional symptoms, including hot flushes, mood swings and vaginal dryness. HRT replaces oestrogen and progesterone which fall as a woman approaches the menopause. As these hormones are replaced whilst using HRT, symptoms can be minimised and bring respite to women who may suffer.
There are 2 main types of HRT, one for if you are experiencing the menopause and another if your periods have stopped completely. The majority of women will take a blend of oestrogen and progesterone, however oestrogen only therapy is available for certain women.
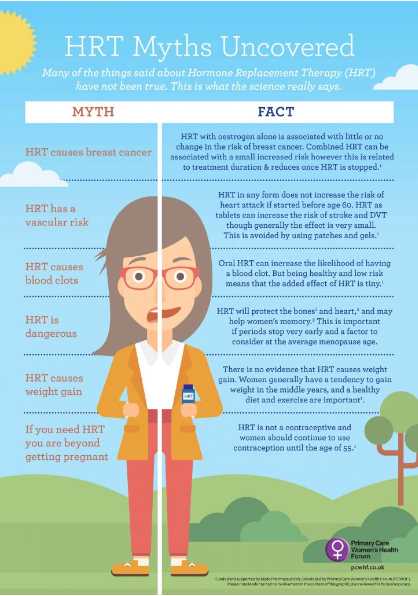
Dispelling the Myths around HRT
There are so many myths and so much confusion around HRT, such as
- HRT causes breast cancer.
- HRT will make me put on weight.
- Taking HRT is delaying the inevitable.
- I suffer from migraines so I can't have HRT.
- You can only use HRT until you are 60.
- And many many more!
We highly recommend that you read up on these myths as they not accurate and are often misleading. Here at BOMIMO, we passionately believe that we need to spread the word that taking HRT is okay for most women and that it literally can change your life by helping you navigate the menopause.
What are the benefits of HRT?
For many women, HRT can help relieve common symptoms that can last up to 12 years from perimenopause to post menopause – for example, hot flushes, night sweats, mood swings, vaginal dryness and reduced sex drive.
HRT can also help prevent osteoporosis (the weakening of the bones), which is more common post menopause.
What are the disadvantages of HRT?
HRT is not suitable for everyone. Women with a history of breast, ovarian or womb cancer, or a history of blood clots, liver disease or high blood pressure, may be recommended an alternative to HRT. There is little to no change in the risk of breast cancer or heart disease if you take oestrogen only HRT, however it does increase the risk of womb cancer, so is only recommended to women who have undergone a hysterectomy. HRT can occasionally cause side effects such as headaches, abdominal pain and vaginal bleeding, which some women prefer to avoid.
When to take Hormone Replacement Therapy?
This depends on your reasoning for starting HRT in the first place and is a very individual decision. If hormone replacement therapy is being used purely for the symptoms of the menopause, generally it can be taken for as long as the menopause symptoms are causing a detrimental effect. If preventing the risk of osteoporosis is a factor in your decision then you need to take HRT for a minimum of five years. Your GP will review the pros and cons of HRT for you every year and any decision to stop should be made with a healthcare professional.
How long after starting HRT do you feel a difference?
It can take a number of weeks for you to feel the effects of HRT due to the low dosage you will start with. If after 6 weeks you have not seen any impact, you may wish to speak to your GP to see if your dosage can be altered.
Types of Hormone Replacement Therapy
There are two main types of HRT:
- Combined HRT (oestrogen and progestogen) – for women who still have their womb
- Oestrogen-only HRT – for women who have had their womb removed in a hysterectomy
There are several ways that oestrogen can be taken, including:
- tablets – which can be taken by mouth
- a patch that you stick on your skin
- an implant – under local anaesthetic
- oestrogen gel – which is applied to the skin and absorbed
- oestrogen spray—which is applied to the forearm
When required to protect the womb lining from being stimulated by oestrogen, progestogen is available as:
- combined with oestrogen in tablets
- combined with oestrogen in patches
- separately as tablets or a progestogen releasing coil
Body Identical Hormone Replacement Therapy

There are so many different types of HRT available. This means that the dose and type of HRT can be altered to suit your individual health needs and risk factors for other conditions, for example if you have had a clot in the past or have high blood pressure. Many women want to take ‘natural’ products for their menopause, but how do you define ‘natural’?
There are many medicines available that derive from plants, so therefore they are ‘natural’, but these are often unsafe and have been shown to be harmful to your bodies. For example, although black cohosh has been shown to have some benefit in the treatment of hot flushes, some types of black cohosh have been shown to be associated with liver toxicity.
Body identical estrogen has the same molecular structure as the estrogen which decreases in your body during the menopause. It is safer to have the estrogen as a patch, gel or spray as this is absorbed directly through the skin and has less side effects and risks. These types of estrogen can be given to women with migraines and those with a higher risk of clot, as there is no increased risk of clot using these types of estrogen. It is also natural because it is derived from a plant chemical that is extracted from yams a tropical root vegetable. Some types of older HRT contain a mixture of different types of estrogens and are made from pregnant mares' urine. This type of HRT could be described as ‘natural’, but it is not body identical as it contains many types of estrogens that you do not need in your body. This type of HRT is rarely prescribed by doctors these days.
There are many different types of progestogens (synthetic progesterone) available for women. If you still have a womb (uterus), it is important that a progestogen is prescribed alongside the estrogen for your HRT. When you take estrogen, the lining of your womb can build up, which can increase your risk of cancer. However, taking progestogen prevents this build up, which means there is no increased risk of cancer when you take HRT. The type of progestogen commonly prescribed is called ‘micronised’ progesterone (Utrogestan). This is a body identical progestogen as it has the same molecular structure as the progesterone in our bodies. This means it is usually associated with fewer side effects than other types of progestogens. Side effects of progestogens can include bloating, spots and mood swings. Micronised progesterone is also made from the yam vegetable. The additional advantage of micronised progesterone is there is no increased risk of breast cancer for the first five years of taking it. After this time, the risks of breast cancer are very low and seem to be lower than the risk for a woman taking the older types of progestogen. All these body identical hormones are usually available on the NHS, although micronised progesterone is not usually available in Scotland.
There is now evidence demonstrating that transdermal estrogen in association with natural micronised progesterone represents one of the optimal HRT regimens. Transdermal estrogen is the preferred route of administration because, in contrast with oral estrogen, estrogen as a patch or gel is not associated with an increased risk of venous thromboembolism. It can be safely given to women who have a history of migraines, gallbladder disease, diabetes, or who are obese. The optimal progestogen is micronised progesterone which is body identical. This usually has less side effects associated with it compared with the older progestogens. In addition, there is no increased risk of breast cancer for the first 5 years of taking estrogen with micronised progesterone.
Testosterone is also a female hormone and often misunderstood. Low testosterone in women can cause lack of energy, brain fog and reduced libido. Unfortunately, testosterone is not licenced in the UK for use by women. But it can be prescribed by a private specialist, some GP's and most menopause experts - but only for low libido. If you are taking HRT and your oestrogen levels are balanced but you are still reporting some symptoms, it is worth investigating testosterone. It is often the final part of the hormone jigsaw.
There are three main options for testosterone available in the UK. Either AndroFeme, Testim or Testogel. AndroFeme is specifically made for women, wherease Testim and Testogel are made for men but can be used by women in smaller doses. Dr Louise Newson has an excellent factsheet on Testosterone
Most women and healthcare professionals are concerned about the possible risks of breast cancer in women taking HRT. However, the risk is far lower than many realise. Women who take estrogen only HRT (women who have had a hysterectomy) do not have a greater risk of breast cancer. The recent epidemiological study did not confirm any additional risks with transdermal oestrogen and micronised progesterone.
Women who take estrogen and a synthetic progestogen may have a very small increased risk of the diagnosis of breast cancer. However, this increased risk is of a similar magnitude to the risk of breast cancer for women who are overweight, or drinking one or two units of alcohol each night. Frustratingly, despite this evidence, only around 10% of women in the UK are currently taking HRT. Although some women choose not to take HRT or cannot take it for medical reasons, a large proportion of women are declined a prescription for HRT for no valid medical reason. This is either because the doctor does not know enough about it and been frightened out of prescribing, or the fact that some practices do not prescribe HRT as a cost saving exercise.
Many women are inappropriately given antidepressants instead of HRT which goes against current guidelines. Often this is due to ignorance (and lack of education) about realising that low oestrogen can cause depressive symptoms. It is increasingly common that women are seeking HRT from other clinics and healthcare professionals to improve their symptoms and quality of life. Over recent years, there has been an increase in the number of private clinics offering compounded bioidentical HRT to women, which is a major concern. These are not the same as the ‘body identical’ hormones or regulated bioidentical HRT.
Body Identical HRT vs Bio Identical HRT
There are very important differences between different types and formulations of HRT. In the past, estrogen in HRT was derived from pregnant mares’ urine. The term ‘bioidentical hormones’ simply means that they have the same molecular structure as the hormones in the body. Regulated bioidentical hormones are usually referred to as ‘body-identical hormones’ (rBHRT) to reduce confusion from compounded bioidentical hormones (cBHRT). Most types of body identical HRT now prescribed are derived from yams, the root vegetable, and are usually available from the NHS, at a cheaper cost than many of the combined oral preparations which contain synthetic progestogens.
The risks associated with Compounded bioidentical HRT
Compounded bioidentical HRT is not subject to any quality control as it comes under a supplement. They often do not have properly enforced standards of good manufacturing, quality controls, and monitoring, as regulated hormones do. Many cosmetic and other types of private clinics in the UK and worldwide are offering these hormones to women, often costing vast sums of money.
The hormones are ‘compounded’ in special pharmacies, so they are custom made to produce tablets, lozenges, and creams, in combination doses or preparations that are not routinely available. These hormone preparations are not subjected to the same tests of safety, efficacy, or dosing consistency, as regulated HRT. These preparations may also contain undesirable additives or preservatives, degradation products, process impurities, residual solvents, bacterial endotoxins, or residual amounts of other drugs made in the same pharmacy.
Of more concern, these compounded hormones often have unsubstantiated claims, lack of scientific safety and efficacy data, and lack of quality control surrounding them. In addition, some of the healthcare professionals who prescribe compounded hormones claim to be able to determine the precise requirements of each woman by undertaking a series of serum and saliva tests. This costly practice has never been substantiated through rigorous research and is not recommended by the menopause societies.
Some of the hormones used in these bioidentical hormones contain hormones that are not approved for women, such as dehydroepiandrosterone (DHEA) or pregnenolone. Many women are given progesterone creams rather than oral preparations, which are usually not well absorbed in the body. There is only very scant data available, but the current evidence has failed to show any endometrial protection from progesterone creams or gels.
There is also a concern with the bioidentical oral preparations, as there may be inconsistencies in the quantities of estradiol and other estrogen preparations in compounded preparations. This can lead to an increased risk of venous thromboembolism, as well as increasing the risk of endometrial cancer.
Compounded bioidentical hormone replacement therapy does not carry the safety warnings for estrogen products that are in all prescribed HRT preparations. These were written after the publication of the WHI study and have not been updated to be in line with current evidence. Understandably, many women are worried about the Summary of Product Characteristics (SPC) currently in regulated HRT preparations, so they falsely think that these compounded preparations are associated with less risk.
Approved, registered, bioidentical regulated hormonal drugs that are produced in monitored facilities are readily available to prescribe for women in the NHS. This means that it is not appropriate or necessary for women to use the potentially harmful, customised, compounded hormones.
It is essential that clinicians and women are made aware of the potential harms of these hormones, and are not enticed into paying money for expensive unregulated products.
How to get started on Hormone Replacement Therapy
Speak to your local GP practice if you're interested in starting HRT.You can usually begin HRT as soon as you start experiencing menopausal symptoms and will not usually need to have any tests first. However, a blood test to measure your hormone levels may be carried out if you're aged 40 to 45. Blood tests may also be carried out to help diagnose suspected premature menopause if you’re under 40 and have menopausal symptoms. Your GP can explain the different types of HRT available and help you choose one that's suitable for you.
Choosing the right HRT for you
It is important to find the correct HRT to help your symptoms. A low dose of HRT hormones is usually prescribed to begin with. If you need to, you can increase your dose at a later stage. Once you've started HRT, it's best to take it for a few months to see if it works well for you. If not, you can try a different type or increase the dose. It's really important that you talk to your GP if you have any problems with HRT.
Shortage of some HRT products
There are ongoing supply problems with some HRT products. For some products this is because of irregular supply while for others it's a longer-term shortage. There are lots of different reasons why medicines can be in short supply. Work is happening with the pharmaceutical manufacturers who make the medicines to help the situation. If your pharmacy can’t supply the specific HRT product you've been prescribed, they may supply an alternative product. This will usually have the same ingredients, but may be made by a different manufacturer. Your pharmacy might also reduce the amount they provide you with to help ensure that as many women as possible can get access to their required medication.
Disruptions in the availability of HRT will be worrying if it has been prescribed for you. However, there are always alternative options. If you are concerned about this, contact your GP, pharmacist or specialist doctor to discuss the best treatment options for you.
When HRT is not suitable
HRT may not be suitable, or a specialist opinion may be needed, if you:
- have a history of breast cancer, ovarian cancer or womb (uterus) cancer
- have a history of blood clots, tablet HRT is not recommended but taking HRT through the skin can be considered
- have a history of heart disease or stroke
- have untreated high blood pressure – your blood pressure will need to be controlled before you can start HRT
- have liver disease
- are pregnant or breastfeeding
In these circumstances, a different type of medication may be prescribed to help manage your menopausal symptoms.
Side effects of HRT
Both hormones used in hormone replacement therapy (HRT), oestrogen and progestogen, have side effects. Side effects usually improve over time, so it's best to try the treatment plan you have been prescribed for at least 3 months. If side effects continue after this time, see your GP so your treatment plan can be reviewed.
Hormones used in HRT can have associated side effects, including:
- fluid retention
- bloating
- breast tenderness or swelling
- headaches
- indigestion
- depression
- vaginal bleeding
If side effects persist, your GP may recommend an alternative treatment plan.
HRT and Weight gain
Many women believe taking HRT will make them put on weight, but there is no evidence that this is the case. You may gain some weight during the menopause, but this often happens whether you take HRT or not. Exercising regularly and eating a healthy diet can help you to maintain a healthy weight.
Understanding the benefits and risks
Recent findings show that although not completely risk-free, HRT remains the most effective solution for helping with symptoms of menopause and is also effective for the prevention of osteoporosis. It may also provide protection against heart disease. Every woman experiences the menopause differently, so there is no way of knowing how long symptoms will last and so how long HRT will need to be taken. Some women who have continued symptoms into the longer term, may need to keep taking HRT to help with symptoms and good quality of life. Further information about the benefits and risks of HRT
When to stop taking HRT
Most women are able to stop taking HRT after their menopausal symptoms finish, which is usually two to five years after they start (but in some cases this can be longer). Gradually decreasing your HRT dose is usually recommended, rather than stopping suddenly. You may find that your menopausal symptoms come back after you stop HRT, but these should pass within a few months. After you have stopped HRT, you may still need help to manage vaginal dryness and to prevent osteoporosis. Read about the best ways to prevent osteoporosis. Cream, lubricants and local oestrogen preparations are available for vaginal dryness and discomfort. You don't need to suffer from vaginal dryness and discomfort without treatment.
What about alternatives to HRT?
If you decide that you do not wish to take HRT, there are a number of alternative treatments and lifestyle changes you can undertake in order to reduce and manage your menopause symptoms.
Have a balanced diet – this ensures a healthy weight is maintained and ensures your bones stay healthy.
Cut down on triggers – alcohol, spicy food and caffeine have all been known to trigger hot flushes – giving up smoking will also help reduce hot flushes, as well as reducing your risk of developing heart disease or cancer.
Regular exercise – this improves sleep and can reduce hot flushes. Physical activity also improves your mental health and can boost your mood if you are feeling anxious or irritable.
Supplements – Supplements, particularly The MenoShake, have been specifically formulated to provide you with the micro nutrients and macro nutrients you provide you with the optimum nutrition you need in midlife, together with herbal supplements known to support women with the symptoms of perimenopause and menopause. The MenoShake is compatible with HRT so can be taken alongside Hormone Replacement Therapy for all round support, or by itself, for women who are unable to take HRT.
See our other blog posts where we provide more information about managing with your menopause symptoms, but don’t be afraid to see your GP if you are having trouble coping

Author: Samantha Williams


Leave a comment
Please note, comments must be approved before they are published